Keeping Rare Melanomas Front and Center: Tebentafusp and
Other Advances

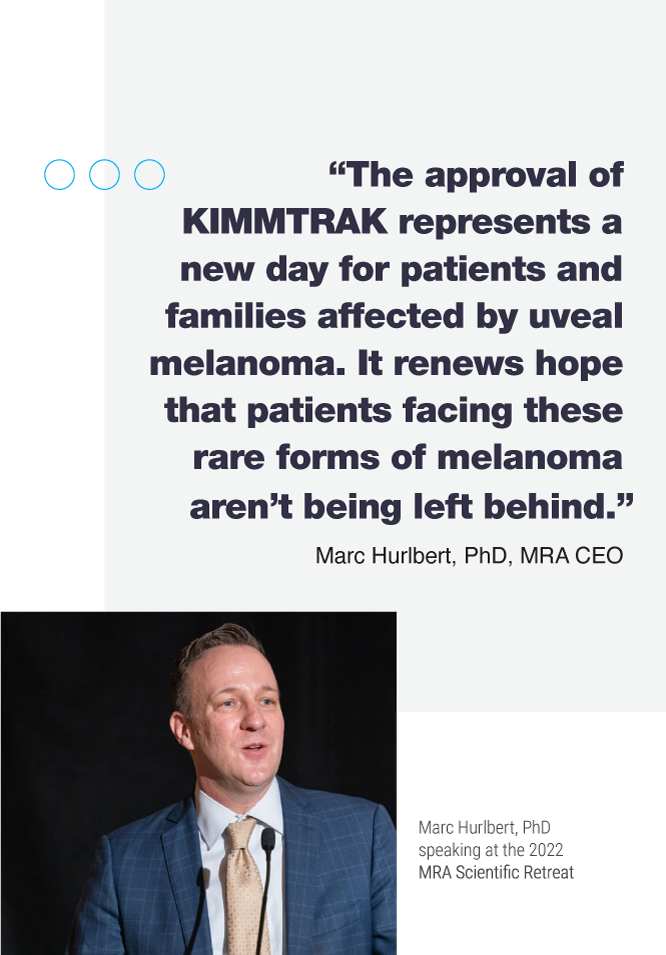
In January 2022, KIMMTRAK (Tebentafusp or “Tebe” for short) became the first-ever Food & Drug Administration (FDA)-approved therapy to treat unresectable or metastatic uveal (ocular) melanoma.
In addition to being the first-ever approval specifically for metastatic uveal melanoma, it is also the first-ever T cell receptor therapy to earn FDA approval for any cancer.
Uveal melanoma, though the most common form of eye cancer in adults, is a rare melanoma subtype responsible for only ~5% of all melanoma diagnoses. Uveal melanoma differs from cutaneous (skin) melanoma in its etiology, the mutations that drive it, and in the patterns of metastases. Moreover, it has now been shown that uveal melanoma and cutaneous melanoma are quite different in the ways they engage with the immune system. As a result, therapies, such as immune checkpoint inhibitors, that have transformed treatment options for cutaneous melanoma do not work as well for uveal melanoma. Thanks to a new clinical milestone and the groundbreaking clinical trials of tebentafusp, patients with unresectable or metastatic uveal melanoma now have a treatment option available. The positive pivotal trial and ultimate approval of tebentafusp has also demonstrated that global randomized clinical studies in rare diseases are possible.
Tebentafusp works using a technology called T cell redirection that brings melanoma cells and T cells closer together to facilitate tumor killing. “It acts like a two-sided magnet that drags the immune system over to something called GP-100 expressed by the melanoma cell,” explains Dr. Marlana Orloff, Associate Professor of Medical Oncology at Thomas Jefferson
University and principal investigator of the tebentafusp clinical trial. “For the ‘magnet’ to engage on the melanoma, it needs to be matched to an HLA type. In the case of tebentafusp, it was developed to interact with the most common HLA type, which is HLA-A201. Therefore, determining a uveal melanoma patient’s HLA type early in their diagnosis is important when making treatment decisions. (Additional information about tebentafusp is available at CureMelanoma.org)
Despite the cause for celebration, Orloff cautions that tebentafusp is not without challenges. For starters, patients who do not have the A201 HLA type do not qualify for treatment: representing approximately half of all patients with uveal melanoma. As such, additional treatment options that are effective for this rare melanoma are still urgently needed. Additionally, tebentafusp requires a weekly infusion with at least the first three doses requiring 16+ hour monitoring period following administration—adding an additional layer of complexity for patients and necessitating increased education for providers to ensure safe administration.
Despite its obstacles, however, Orloff is hopeful that what the field has learned through tebentafusp’s development may eventually help other hard-to-treat patient populations, such as patients with cutaneous melanoma who are resistant to standard checkpoint immunotherapy or who haven’t responded well to immunotherapy because, perhaps, under the surface their melanomas have more similarities to uveal melanoma.

“I think the time has come where maybe cutaneous melanoma and the cancer field at large can learn a bit now from uveal. I think the investment in research into uveal melanoma, even though it’s a rare melanoma subtype, can hopefully be brought into the other more common melanomas and other cancers,” says Orloff.
Orloff credits funders like MRA with helping keep rare melanomas front and center. In fact, about 10% of all MRA grant awards have focused specifically on rare melanoma subtypes. Orloff, an MRA-funded investigator, says, “MRA has been great in having specific funds in every award cycle dedicated to rare melanoma subtypes. At the Scientific Retreat, MRA will often give the stage to me or other melanoma medical oncologists who specialize in treating patients with rare subtypes, so that we can present our work and get the word out. When tebentafusp was approved, MRA reached out to me immediately and did a great job sending that information out broadly.”
In addition to tebentafusp, other interesting research is taking place in the uveal melanoma space, including those designing therapies targeting mutations common in uveal melanoma, called GNAQ and GNA11. At Thomas Jefferson University where Orloff works, the team is exploring several novel approaches to liver-directed therapy, the most common site for uveal melanoma metastasis. “A unique feature of uveal melanoma,” says Orloff, “is that the cause of death for close to 90% of patients is liver failure due to extensive hepatic involvement by tumors. By exploring novel approaches to treating liver metastases and conducting clinical trials in this area, we will hopefully broaden our toolbox even further for our uveal melanoma patients.”
Orloff adds, “Before this year there were no uveal melanoma treatments but now, with tebentafusp, the dam has been breached. I’m hopeful that it is the first of many treatment options to come. This is by no means the end. Instead, this is just the beginning.” ![]()
Advancing RARE Melanoma
Research, Together
Advancing RARE Melanoma
Research, Together
In addition to uveal melanoma, MRA is also focused on accelerating research into other rare melanoma subtypes.
In 2022, MRA launched the RARE Registry, a new direct-to-patient effort to advance research focused on acral and mucosal melanoma – two rare and difficult-to-treat subtypes of the disease. MRA’s RARE Registry complements existing patient registries focused on uveal melanoma.
Patients with these acral and mucosal melanomas, like those facing uveal melanoma, are often the only—or one of very few—patients at their clinic with this diagnosis. This has made it difficult for patients to connect and share information as well as for researchers to access the clinical information, tissue, and genomic profiles that they urgently need to better understand the causes and possible treatment options for these rare melanoma subtypes.
To address this, MRA began work in 2020 to develop the RARE Registry, a bidirectional and interactive registry for patients facing acral or mucosal melanoma. Through RARE, patients and families affected by rare melanomas will have a platform to build community and researchers will gain critical insight into the risk factors, treatment histories, and unique experiences of patients facing these subtypes to drive research forward.
